Do you know how to handle chemical burns? Do you have a mandatory 20-minute on scene flush policy?
Having had the opportunity to travel nationally, teaching hazardous materials response and prevention for over 25-years, I became aware that there was a common thread between many different firefighters that I spoke to during class breaks. All of them candidly shared that when they were exposed to a hazardous material, both their medics and the hospital were ill prepared to deal with their injuries... but they promised to do better next time.
In an effort to prevent any of you from becoming Guinea Pigs... I share this Standard Operating Guideline that was written years ago by the Santa Clara County EMS Authority.
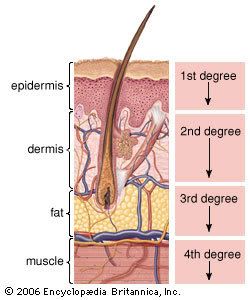
Burn Review:
Here's the example that was shared during the seminar:
Scenario One: A young child hears a knock on the front door and goes to the door to answer it. After opening the door, a familiar figure stands there with a glass jar filled with liquid. The stranger was the step-father taking revenge against his ex-wife on the child. One gallon of hydrochloric acid was splashed directly into the childs face and chest. 911 was called and within minutes an engine company pulled up on scene and evaluated the scene.
Immediately, the Fire Captain grabbed the kid by the back of the neck, took him out to the front yard and followed a new policy taught to the fire department by nurses from the local emergency room. The policy was simple, anyone exposed to a liquid corrosive hazardous material shall be flushed for a minimum of 20-minutes, on scene.
About 10-minutes into the incident, an over zealous private ambulance company medic insisted that he take the patient immediately to the hospital. The Captain did not relent his hold on the kid or the flow of water flushing his eyes and face. The more insistent the medic became, the more the Captain felt any degree of patience. The medic was eventually arrested under protest and placed into the back of a patrol car.
The child was released 10-minutes later by the fire department and was transported to the local hospital. The child was released 2-hours later with no injury, burns or damage to his eyes, all because the fire department followed these standardized rules for chemical exposure.
The solution to pollution is dilution. Anyone exposed to a hazardous materials needs to be evaluated as soon as possible but if they have chemicals on them, you need to ensure that as much of the chemicals have been flushed or vacuumed off prior to transport to a medical facility.
Scenario Two: A worker accidentally falls into a vat of sodium hydroxide (Lye). In the excitement , a helicopter is dispatched to the scene to immediately get this man to the hospital. Emotions were raging and to protect the pilot and crew from exposure, the victim was placed into a body bag to prevent secondary contamination. When they arrived at the hospital, the victim had expired and had suffered fourth degree burns.

Immediate decontamination makes sense using the 20-minute on scene flush policy.
Discuss this concept with your local EMSA (Emergency Medical Services Agency) if you do not have this guideline as one of the tools used to minimize the damage caused from these types of exposures.
Being expedient about providing the flushing is paramount if you are going to make a difference. Couple this with the elderly or small children and the results may prove to be fatal.
Remember that with corrosive burns for example, what is happening is that you are first off getting an exothermic reaction which is the generation of heat that causes the actual chemical burns. Secondly, the chemicals break down intercelluar walls and get transported via your lympatic system to other parts of the body. The sooner the chemical(s) are removed the better chance your patient has of surving this insult and will suffer a lesser degree of burn.
The life you save may be your own...
Stay safe,
Mike Schlags
Santa Barbara, CA
mschlags@yahoo.com
In an effort to prevent any of you from becoming Guinea Pigs... I share this Standard Operating Guideline that was written years ago by the Santa Clara County EMS Authority.
Burn Review:
Here's the example that was shared during the seminar:
Scenario One: A young child hears a knock on the front door and goes to the door to answer it. After opening the door, a familiar figure stands there with a glass jar filled with liquid. The stranger was the step-father taking revenge against his ex-wife on the child. One gallon of hydrochloric acid was splashed directly into the childs face and chest. 911 was called and within minutes an engine company pulled up on scene and evaluated the scene.
Immediately, the Fire Captain grabbed the kid by the back of the neck, took him out to the front yard and followed a new policy taught to the fire department by nurses from the local emergency room. The policy was simple, anyone exposed to a liquid corrosive hazardous material shall be flushed for a minimum of 20-minutes, on scene.
About 10-minutes into the incident, an over zealous private ambulance company medic insisted that he take the patient immediately to the hospital. The Captain did not relent his hold on the kid or the flow of water flushing his eyes and face. The more insistent the medic became, the more the Captain felt any degree of patience. The medic was eventually arrested under protest and placed into the back of a patrol car.
The child was released 10-minutes later by the fire department and was transported to the local hospital. The child was released 2-hours later with no injury, burns or damage to his eyes, all because the fire department followed these standardized rules for chemical exposure.
The solution to pollution is dilution. Anyone exposed to a hazardous materials needs to be evaluated as soon as possible but if they have chemicals on them, you need to ensure that as much of the chemicals have been flushed or vacuumed off prior to transport to a medical facility.
Scenario Two: A worker accidentally falls into a vat of sodium hydroxide (Lye). In the excitement , a helicopter is dispatched to the scene to immediately get this man to the hospital. Emotions were raging and to protect the pilot and crew from exposure, the victim was placed into a body bag to prevent secondary contamination. When they arrived at the hospital, the victim had expired and had suffered fourth degree burns.

Immediate decontamination makes sense using the 20-minute on scene flush policy.
Discuss this concept with your local EMSA (Emergency Medical Services Agency) if you do not have this guideline as one of the tools used to minimize the damage caused from these types of exposures.
Being expedient about providing the flushing is paramount if you are going to make a difference. Couple this with the elderly or small children and the results may prove to be fatal.
Remember that with corrosive burns for example, what is happening is that you are first off getting an exothermic reaction which is the generation of heat that causes the actual chemical burns. Secondly, the chemicals break down intercelluar walls and get transported via your lympatic system to other parts of the body. The sooner the chemical(s) are removed the better chance your patient has of surving this insult and will suffer a lesser degree of burn.
The life you save may be your own...
Stay safe,
Mike Schlags
Santa Barbara, CA
mschlags@yahoo.com
Tags:
Replies to This Discussion
-
Permalink Reply by Benbesher on January 27, 2011 at 9:46am
-
hi Norm, you said that " if the material is a dry chemical brush as much off as quickly " but you didn't tell us how and what we have to use or have to avoid to do, cause you know with the panic some people could make things worst.
thanks.
-
Permalink Reply by Mike Schlags (Captain Busy) Retd on January 27, 2011 at 10:43am
-
No, I think we are moving back to common sense Ralph. There are just some circumstances where you need to load the patient and do your best to stabilize them enroute, shortening as much as possible the length of time it takes for a victim to receive in-hospital advanced care. This is how people survive, not by having paramedics evaluate and do basic procedures in the field.
-
Permalink Reply by Mike Schlags (Captain Busy) Retd on January 27, 2011 at 11:01am
-
And if the material is a dry chemical brush as much off as quickly as possible before irrigating.
IMPORTANT: This is REALLY true if the chemical is on the patients face. Protecting the airway and the sensitive eye tissues is paramount. Always place a dust mask on the victim as soon as possible.
Engine Company Response: Removing as much of the product, without creating dust by brushing needs to be accomplished in conjunction with removing the contaminated clothing. Making sure that none of the chemical makes intimate contact with the skin is your number one goal. Remember, if you have to do this procedure then you have to assume that the area will become contaminated. If you have a tarp to do this procedure on, you will save a lot of hassle later... Once the dry materials are off, you have to make the subjective call whether or not to initiate emergency gross decontamination. If the victim or people, if it's a mass casualty incident (WMD), and folks are complaining about burning in the eyes, arm pits, mouth, then it's pretty safe to conclude that you need to use a lot of water to dilute what ever has compromised the health and safety of the patient or public.
Hazmat Team Response: Brushing things off should not be the treatment of choice if you are doing actual decontamination. Using a HEPA vacuum cleaner would be preferable (like everyone has one...) because it would not vaporize and distribute the dry/fine particles for the involved chemical (more exposure potential + more contamination = we are not suppose to make things worse).
For both ambulatory and non ambulatory decontamination, clothing has to be removed safely. This can be done by rolling the clothing off, trapping debris and chemical as you roll the clothing, in conjunction with a pair of scissors to cut away material. Remember that until told otherwise, you need to safely bag and tag any removed clothing for both contamination issues as well as evidentiary issues should it be a terrorist action or a crime scene.
CBz
-
Permalink Reply by Mike Schlags (Captain Busy) Retd on January 27, 2011 at 12:24pm
-
Ben, My above reply does not include specifics on what you would use to accomplish this type of decontamination. First off, if you have nothing but your gloved hands, then that will work. Protecting yourself first and then prioritizing the patients airway are your number one concerns upon contact with a victim.
As far as tools beyond vacuum cleaners, if you have a soft paint brush, then you can gently brush away particulates and dust. My comments about use of a special type of vacuum cleaner is still the best option if available. I say this because fire prevention folks or whoever permits the fixed facility that stores, uses, handles or transports on site can require, by Uniform Fire Code, appurtenances to provide enhanced emergency preparedness. This can include fire extinguishers, fire hose, ventilation or even special vacuum cleaners should an employee be exposed. Just sayin'
There is no question that tepid water (not too hot or too cold) combined with a mild surfactant (soap) is the best approach to decontamination. The concern expressed here is for solids that when exposed to water, turn into something else. Sulfur plus water equals sulfuric acid... Nasty stuff.
If it's liquids involved then this discussion is moot. Lot's of water combined with removing the contaminated clothing enables folks to pretty much remove most of what it was that contaminated them without incident because the contamination is on the outside of the persons clothing. Primary contamination points for everyone are the hands and feet with the face being the primary concern due to respiratory concerns.
CBz
-
Permalink Reply by Seth Malcolm on January 27, 2011 at 1:31pm
-
What you guys are saying is so true. I would like to add that some of your haz-mat team are firefighters better have a EMT-B are higher to start pt care, if they don't then thats something that may need to be look at on a department level. Some agents cause more than burns and they need more than flushing. This is where FD and EMS MUST work hand in hand so everyone goes home. The cert level in am area is a big deal because most of the FD are vol. and thats great, but we need to know what best for the pt. I for one will not pt a pt in my box that I know has been in HAZ-MAT untill decon has been done. So I guess what I am sayiing is JOINT COMMANED....
S Malcolm
-
Permalink Reply by Mike Schlags (Captain Busy) Retd on January 27, 2011 at 1:51pm
-
Your gut feeling is right on the money Seth... NO ONE should be placed into the back of an ambulance that has not been decontaminated completely. And yes, the fire department and the EMS provider have to work together because some exposures dictate antidotal treatments and if the EMS folks are the ones with the drugs, it stands to reason that we need to enable patient care to prevail as the priority. One problem is that the patients have to be fully decontaminated before the EMS folks can have access. This is one of the benefits of having a firefighter paramedic at the victims side from the very start.
One problem to contend with is that not all states have standardized poison antidote treatments for paramedics to follow. Nor does everyone have access to the antidotes. This is why it is important for the fire department to preplan worst case scenarios, which includes researching MSDS data on site to see if there is anything special that needs to be planned for in the event of an emergency.
- ‹ Previous
- 1
- 2
- Next ›
Specialty Websites
Find Members Fast
Firefighting Videos
© 2026 Created by Firefighter Nation WebChief.
Powered by
![]()
Badges | Contact Firefighter Nation | Privacy Policy | Terms of Service